How a Nobel Prize winner in economics informs our Self-Health Care
I have a reframe for you. It's inspired by the Nobel Prize-winning Israeli-American economist and Princeton University professor emeritus Daniel Kahneman. That's a prestigious mouthful, I know. And you may be wondering how an economist can help you with your self-health care. But I promise you that if we borrow from theories that Kahneman has proven, it will inform how you become a leader in your own healthcare. You call the shots. You know your direction of care. And your health and medical teams work for you.
If this seems impossible from where you're sitting, I beg you to read on.
Acute and Chronic, what's the difference (and why does it matter)?
First, we need to define two key terms that have as little to do with Kahneman's principles as healthcare does. Stick with me here, as these definitions will help us find our way into this economically sound reframe that'll help you step back into the driver's seat of your own care. The two terms we're exploring are acute and chronic.
Acute:
1. very serious or severe
There is an acute shortage of water.
acute pain
the world's acute environmental problems
acute competition for jobs
2. an acute illness is one that has quickly become severe and dangerous
acute appendicitis
Chronic:
1. (especially of a disease) lasting for a long time; difficult to cure or get rid of
chronic bronchitis/arthritis/asthma
the country's chronic unemployment problem
a chronic shortage of housing in rural areas
2. having had a disease for a long time
(source: Oxford's online Learner's Dictionary)
While I'm guessing these definitions are nothing new to you, we've lost sight of their potency when thinking about healthcare. And when I say "we," I don't just mean you and me. I also mean the systemic structure in which we are delivering care. Part of the issue is that we, as patients, are looking for resolutions to our chronic health challenges in a paradigm that is expertly designed to address acute health concerns. In addition, those that serve the current structure (meaning most healthcare practitioners) are so well trained in delivering solutions for acute issues that they've largely lost the skill of thinking differently and addressing a chronic challenge or condition.
Seeking help for chronic health concerns in traditional or allopathic care is a tragic mismatch. And there's no wonder that frustrations with our medical system run rampant.
Let's step back and identify what an acute health challenge might be…
a broken bone
an asthma attack
a heart attack
a burn
pneumonia
the flu (or a virus)
a respiratory infection
food poisoning
strep throat
a burst appendix
You get the picture. An acute illness or injury occurs suddenly, with rapid onset. Depending on its severity, it usually goes away on its own or with some targeted health or medical interventions. And, as is the case with a heart attack, it could be life-threatening without the appropriate medical care. When you call your doctor after hours, the message will likely say: "If you believe that you are experiencing a medical emergency, please hang up and call 911 immediately or proceed to the nearest emergency room or after-hours medical facility." This is because acute issues need what Kahneman calls "fast thinking."
Can we just take a moment to celebrate the fast-thinking put into action in our emergency rooms, by paramedics, during surgical processes, and so many modern-day medical personnel and procedures? The construct leading to the grievances saves lives, predominantly when attending to those acute concerns it's designed to address.
Thank you, modern medicine!
But, how about a chronic health concern? Let's take a look at some examples of these…
high blood pressure (not induced by "white coat syndrome")
diabetes
arthritis
depression
osteoporosis
cancer
heart disease
Alzheimer's
autoimmunity
PASC (post-acute sequelae of SARS-CoV — i.e. "long-haul")
The list can go on and on, of course. But that last bullet point says it all! This chronic condition is "post-acute." And this can be true of all acute conditions: they can lead to more chronic health challenges if not properly or fully addressed or resolved at the time of their relative onset — becoming post-acute.
A chronic condition typically has a slow progression that builds over some time. While there may have been one trigger (like one of those acute conditions listed above), that one trigger likely occurred in a field where other underlying factors allowed that isolated insult to provoke a long-lasting problem. Most acute stimuli do not become chronic without a permissive biological landscape.
Epstein-Barr Virus… when the acute becomes chronic
An example of the potential for the acute to become chronic (or "post-acute") is the virus called infectious mononucleosis (IM). Upwards of 90% of adults in America are said to have been infected with IM by the time we are 35 years old, with primary infection usually occurring in our childhood, young teens, or early 20s. IM manifests with signs of fever and swollen lymph nodes and symptoms of fatigue and sore throat. The incubation period is between 3-6 weeks, making exposure challenging to pinpoint. While several viruses can lead to IM, the most prevalent is the Epstein-Barr virus (EBV), which makes up about 90% of IM cases.
Even once the symptoms of the infection go away, EBV stays in the body in its inactive form in perpetuity. Its ability to cause symptoms is controlled by complex mechanisms of our highly adaptive immune system. Yet EBV can reactivate without us even knowing it, enabling us to transmit it to others, unbeknownst to us (or them). It can also get chronically stimulated for those of us who cannot control the reactivation of the virus. This can happen when our immune system is triggered or compromised for one reason or another. Common triggers for EBV reactivation include heightened stress, toxins (such as mold exposure), other infections, hormone imbalances, or immunosuppressant agents.
When this happens, we may be facing what's called chronic EBV. There's been a slow progression of the viral activation in a terrain (including any combination of stress, toxins, infections, hormone imbalances, etc.) that enables a virus to proliferate and an immune system to struggle beyond its one-and-done acute function. And the signs and symptoms of that biological burden, from extreme fatigue to nerve impairment, rob you of your everyday ability to do what you are meant to do.
The problem: We're still looking to the "fast thinking" model for what requires an alternate approach! And this is where Kahneman's principles of "slow thinking" deserve our attention, especially when it comes to our self-health care.
Acute health problems demand "fast thinking," but chronic health challenges require "slow thinking"
In Kahneman's book Thinking, Fast and Slow, he defines two ways we think through problems. System 1 thinking is quick, automatic, and often impulsive. System 2 thinking is analytical and deliberate. System 1 thinking is fast and necessary for so many everyday activities, and urgent, on-the-spot, and acute situations. Yet bringing System 1 thinking to System 2 problems that demand a different thought process is sloppy. And when we do try to use System 1 thinking for System 2 issues, we often recruit cognitive biases to legitimize our approach. Whether our choices are right or wrong, we’ll find ways to favor our opinion and justify our actions.
Confirmation bias is one heuristic we may experience with our healthcare providers when they employ System 1 thinking. This can occur when they see your case only through the lens of a particular diagnosis or test result. Instead of embracing the whole, they selectively focus on specific data points in your health history or labs to confirm their belief while ignoring or overlooking other vital elements of your story and experiences.
And we, as patients, may often fall prey to what Kahneman calls the planning fallacy. This is a bias where we underestimate the amount of time needed to address a chronic condition. Because we are thinking with an acute care mindset (or caught in what I often call the "quick-fix trap"), we expect more immediate results than is realistic. If it took a long time to get here, it might also take more than a minute to reverse.
How to apply "slow thinking" to your chronic health challenges
If you're along for the ride, know that we’re about to go slow. As Shakespeare said, “Wisely, and slow. They stumble that run fast.” We’ll smell the roses and stop to pick daisies. None of that can be done going 80 miles an hour.
Step 1:
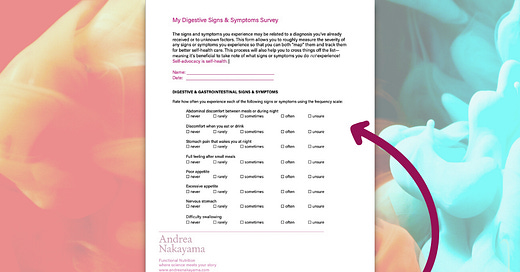
Download the My Digestive Signs & Symptoms Survey
Step 2:
Complete the Survey to the best of your ability.
Step 3:
Go back through and highlight the signs or symptoms that you've been struggling with for a year or longer.
Step 4:
Pick one or two from that list of more chronic signs or symptoms and think back over your history experiencing them. Has anything helped that symptom to feel better or made it feel worse? If so, make a note right on the sheet or somewhere else you keep notes for yourself.
Step 5:
If you identified something (or things) in Step 4 that fell into either the “better” or “worse” category, consider what you might shift that allows you to bring some of Kahneman's "slow thinking" to your health challenge.
Step 6:
Let me know! Is there a place that System 2 thinking (i.e. “slow thinking”) has worked in your health or your life? Is there a place that you’d like to apply it? And if you need help figuring out how to apply slow thinking to a chronic digestive issue, let me know that too!