We now know how rampant medical gaslighting is. There are books on the topic. Mainstream media is popping up with Opinions and stories. Just last week, my childhood BFF sent me an article from the NY Times with the note, “you could have written this.”
Medical gaslighting can make you feel minimized, unheard, misunderstood, dismissed. Maybe you start second-guessing yourself. That sucks. Yet it’s even worse when your provider is unable to recognize the needs of those who occupy bodies different than their own – whether the differences are due to gender (or gender norms), sexuality, race, class, culture, body size, identity, or situational circumstances.
“If any female feels she need anything beyond herself to legitimate and validate her existence, she is already giving away her power to be self-defining, her agency.”
- Bell Hooks
All bodies can suffer from discomfort, dysfunction, and dis-ease. Kidney failure, cancer, and Hashimotos don’t discriminate. Nor does any other illness.
It’s crushing to know that health and medical providers can help, but sometimes do not. And so I find myself awkwardly fumbling my way out of the exclusivity of the field I love and the modalities I believe in (Functional Medicine, Functional Nutrition) to explore access. I trust the Functional approach. We all deserve this kind of care. Yet I’m tired of seeing it restricted to those with the means to know it exists or those who can afford concierge services and a battery of tests (that may or may not be necessary).
Nutrition need not be a dirty word
I don’t believe that Functional Nutrition needs to be expensive (or offensive – as “nutrition” seems to have become – in an age where we ditch the diet and reclaim our bodies and desires). I do not believe in conducting all the testing before it’s clinically time to do so. I do believe in the democratization of Functional Nutrition – in exploring how we all find the Functional Nutritionist in our own back pocket. And this is where I stumble and trip, learning what it means to be an advocate for care, especially for those who are sick and not getting better. It requires patience, humility, empathy, and a good ear. It takes caution, vulnerability and compassionate leadership to offer what I know about the body and its healing potential, even when these discussions are complex, nuanced, and sometimes political.
As I think through my tips for moving beyond gaslighting, I consider: are these tips only relevant for those who were gaslighted and then had the resources to find the provider who would become their savior? (If that’s you, you are very fortunate!) Or can I design them for those for whom gaslighting is expected and baked into their personal or familial history? I know the answer. And I admit that I may not know all the answers. I cannot know all of your experiences. But I do ask you to try these steps on for size, as I discuss them this month, and to speak up and let me know if I missed something that is true for you.
So what’s next after those incidents that leave us feeling like we need to legitimize and validate? How do we move beyond the anger and frustration of not being able to trust a healthcare provider to do what we thought they would/should/could do? And more importantly, how do you overcome the possible disappointment in yourself for not trusting your gut as quickly as you wish you had?
I have a lot of feelings about how we’re looking to medicine and certain medical professionals for the wrong things, but before I go there, let’s talk about us… the patients. Because let’s be real, nobody will take care of you like you.
As you consider those steps, which I promise I’ll explore in more detail, we need to acknowledge that stories of medical gaslighting sit on a spectrum. The experience I shared last week was little ‘g’ gaslighting, but it woke me up. Unlike intimate gaslighting, which often stems from narcissism and abusive intentions, medical gaslighting is usually more naive. It comes from
lack of knowledge
limited understanding of the contributing factors of illness beyond what can be “fixed”
insufficient time (or other resources) for empathy, or
potential distrust of the patient experience
In other words… it’s not about you.
Until it is.
Adrenal Fatigue was not the answer
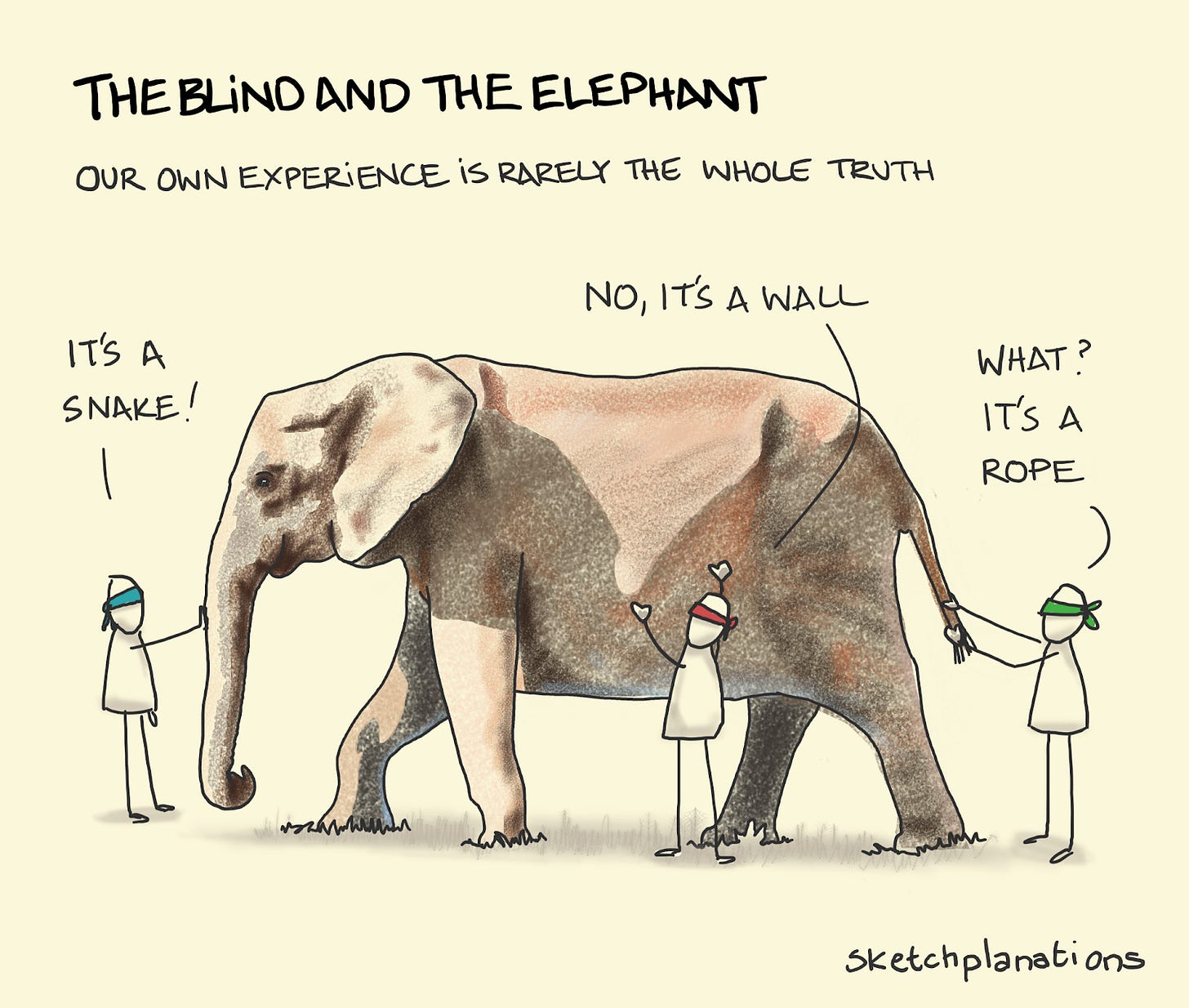
Once again, it was about me when I went to the naturopathic doctor asking what was happening in my body several years after my husband died. This was way back when the diagnosis du jour was “adrenal fatigue”. In my 15+ years in the healthcare space, I’ve seen this zeitgeist shift plenty of times. Parasites. SIBO. Candida. Mold Toxicity. Heavy Metals. Heck, people used to claim their MTHFR was the root of their problems and point to their SNPs as a diagnosis. I’m not saying those things don’t exist or that they don’t play a role in health outcomes. They do! Yet I have issues with clinicians who get hooked on these conditions, diagnosing all patient problems through that lens alone. Like the parable of the three blind men touching the elephant, this can become a quest to confirm bias. (Isn’t one sign of a good scientist to prove yourself wrong, not right?).
The well-meaning ND that I saw heard my story: the loss of my husband, raising a small child, putting myself back through school, and a full-time job. From this she determined (without testing in a circumstance where I would have welcomed it) that I had adrenal issues. She prescribed a supplement regime based on the supposed diagnosis.
The results were bad. I could not get out of bed while on the prescribed nutraceutical plan. Her response: “this is what you have to go through in order to improve.”
That right there is a form of medical gaslighting. I shared my experience and it was dismissed. In fact, the truth of my situation (my adrenals were fine and I had the onset of autoimmune thyroiditis), was never properly assessed until much later. I was seen as a young “widow”, a single mother, a driven woman, and treated for that. My history was heard, but not placed in the context of my concerns for long enough to establish an appropriate diagnosis. Again, I want to recognize that there are a spectrum of medical gaslighting situations that escalate all the way up to a capital MG, many of which I’ve witnessed firsthand in my years in practice. But I want to consider how we shift the power and truly start to get our health needs met.
You too?
Tune-in
I invite you to sit with the three steps listed above. If you have a moment in your own personal history that you can define as medical gaslighting, tune in to where it sits in your body. How does it impact your relationship with medicine, health care, or even yourself?
Next week we’ll kick off by exploring how to move through the steps so that we can all do a little spring cleaning of these toxic experiences.





When I was 13 I was diagnosed with hypothyroidism at 16 they removed my thyroid and I had to take leviothyroxine and I spent the next 42 years battling obesity, pre-diabetes, skin problems and chronic constipation all based on every trip to the doctor and being told "you have no thyroid you will always struggle". Yes I am a work in progress but once I had corrected my nutrition, gut issues and blood sugar issues I lost all the weight but I did that on my own no doctor ever helped I think I have been medical gas lighted more times than I have had hot dinners, it's shameful. I hope never to let my clients down.